Don’t live in denial. Actionable tips to tackle and zero down on claim denials
- SolvEdge
- Dec 01, 2022
- 4 mins read

Claim denials have hit record high levels in recent times. Consider these facts—Denials in healthcare have increased by a staggering 23% in 2020 compared to four years ago. 33% of hospitals are reported to be “exceeding the danger zone” with an average claim denial rate of 10%. This in turn has a significant negative impact on the operational costs and efficiencies of healthcare organizations.
Reworking claims alone cost 20% of the overall healthcare revenue cycle operational expenses, with an average claims rework cost of $25 per claim. From key challenges to major denials in medical billing, in this blog we get to the root cause of denials, provide a strategic approach to reduce & prevent denials—and ensure that you collect every dollar due!
Let’s DIVE IN.
Amidst these alarming industry reports and challenges, the good news is that 90% of claim denials are preventable. Here’s how care providers can significantly reduce denials, lower costs and increase revenues—by having a strategic approach to denial prevention.
Root Cause Analysis: A Strategic Top-down Approach to Denial Prevention
A standard denial management process can provide ad hoc solutions to some of the pressing denial challenges that need immediate intervention. However, for a more effective denial prevention strategy, you need to get to the root of the issue.
Root cause analysis is a significant step in denial prevention. Several hospitals and practices leverage the capabilities of claim management software with automation solutions to simplify and improve efficiencies of the denial management process. Consider asking these critical questions to start with.
10 Questions to Ask in Determining the Root Cause of Denials
What are the key reasons for denials in your Practice?

Segment and
Prioritize Denials
Prioritize Denials
It is also best practice to create benchmarks to rein in denials and improve denial ratio.
Once the root causes are identified, segment and prioritize denials—to determine the causes that have the most impact. Identify vulnerabilities in the current denial management process. Segmenting denials into buckets accelerates the time spent on resolving them. It can bring to the surface denial patterns and common denominators that lead to denied claims. Prioritize denials based on dollar value and TFL.

Segment and
Prioritize Denials
Prioritize Denials
Once the root causes are identified, segment and prioritize denials—to determine the causes that have the most impact. Identify vulnerabilities in the current denial management process. Segmenting denials into buckets accelerates the time spent on resolving them. It can bring to the surface denial patterns and common denominators that lead to denied claims. Prioritize denials based on dollar value and TFL.
It is also best practice to create benchmarks to rein in denials and improve denial ratio.
Denial Prevention Strategies Specific to Eligibility
Eligibility denial is the topmost reason for denials in healthcare—contributing to about 30% of the overall denials in medical billing. Your root cause analysis may help reveal the intricacies of the eligibility specific denials. For instance, it may be due to the negligence of administrative staff in performing a thorough eligibility verification. To fix this, you can verify the eligibility at regular and specific intervals—once during online scheduling—three days prior to the doctor’s visit, then on the date of service, and again before submitting the claim. However, for emergency visits, patient eligibility verification needs to be handled differently at Point of Service—in a way that offers the best medical and financial advice on various care plans.
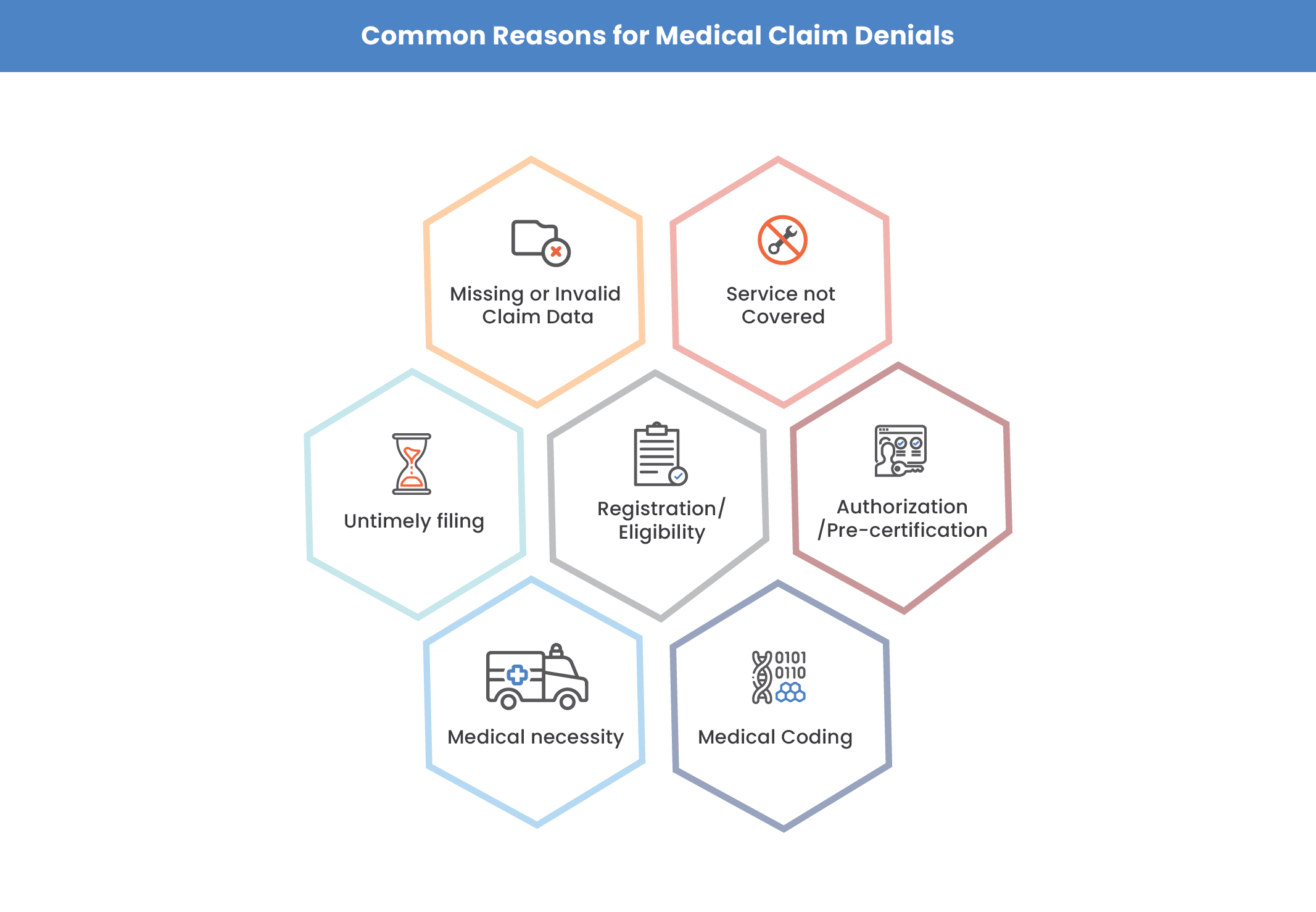
Claim denials in healthcare could be attributed to several factors including—missing or invalid claims data (17.2%),
pre-authorization/pre-certification (11.6%), service not covered (10.6%), medical necessity (6.6%) and so on. That’s why, our team of denial management service experts at SolvEdge has strategized the 4Clover program for denial management (a phased approach that includes—1. Analyze, 2. Strategize, 3. Discover & 4. Implement) to reduce and prevent denials from the ground-up.
SolvEdge’s Denial Management Services
Our denial management services and strategies are uniquely designed to reduce spiking denial rates, while having a proactive approach to denial prevention. Our customized workflows help determine the root cause of denials. Once the denial patterns are identified, we create a detailed report that evaluates the recurring causes of claim denials under various categories. By leveraging these insights, we implement process improvements to reduce denials and optimize revenues.

Get your personalized and free consultation on how SolvEdge’s denial management services can help reduce your denial percentage and drive up your revenues and cash flow
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading healthcare services and solutions provider—trusted by 450+ Hospitals.
