Value-based Revenues – Key
Maximizing Value-based Revenues – Key Tactics You Don't Want to Ignore

Blog
Maximizing Value-based Revenues – Key Tactics You Don't Want to Ignore

Here’s why it will be. Health insurance companies cannot afford the rising cost of care, especially in case of chronic illnesses.
C Changing regulations are creating a transformational impact on the healthcare landscape. One of the key areas evolving is the fee-for-service payment models. Reports suggest that the Fee-For-Service or the FFS model is an established healthcare payment structure, which is soon to become obsolete. Here’s why it will be. Health insurance companies cannot afford the rising cost of care, especially in case of chronic illnesses.
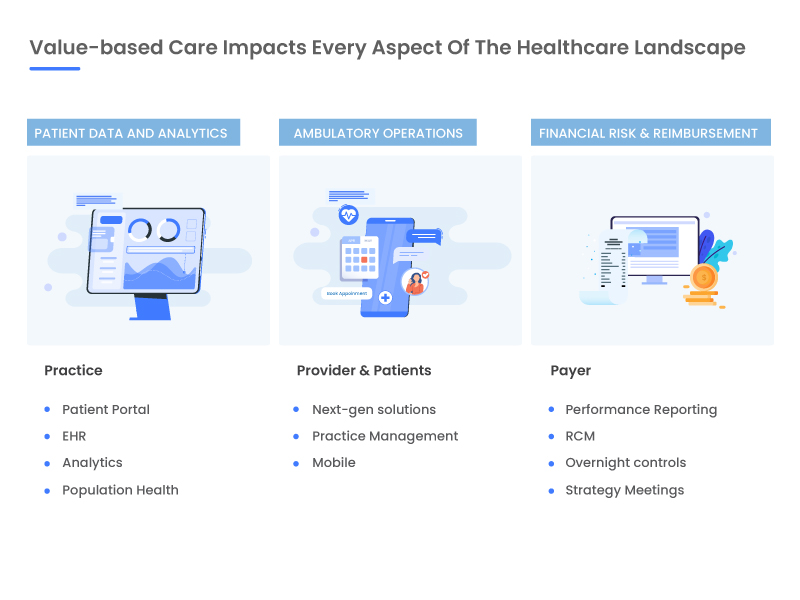
Value-based payment models are associated with improving patient outcomes and reducing the cost of care delivery. Value-based care encapsulates various factors including Pay for performance (P4P), Risk-sharing, Incentivized payments, Capitation arrangements, Gain sharing, Value-based purchasing, Risk-adjusted care, and Population-based payments.
Having a proactive care approach rather than reactive, at a lower cost are some of the key factors that contribute to the success of value-based care. Hospitals and practices need to focus on population health management, reducing hospitalizations and readmissions, improving patient outcomes at a significantly lower cost. This will result in increased cash flow and revenues for providers based on the health outcomes of the consumers.
To achieve success, care providers need to realize the importance of patient-centered care coordination solutions. This fosters collaborative care and can be achieved only through automation and insight-driven healthcare.
Based on an organization’s willingness to take risks, care providers can consider choosing from different payment models that can be integrated into their workflows. One of the most adopted models include the Shared Savings approach that requires providers to effectively manage costs, while delivering high-quality care, for which they will be appropriately rewarded with a part of their savings. Alternatively, providing high-cost and inefficient care could have detrimental effects on the provider through the means of additional costs and penalties. There are few other models that you can choose from in terms of the risk factors:
The triple aim of healthcare comes down to these - improve health outcomes, deliver better quality healthcare, and drive down the cost of care.
Keeping in mind the overall goal of a value-based delivery model is to improve key performance indicators across the care spectrum, Payers make this possible with changing models on how providers are compensated for care delivery, in terms of cost, time and quality.
Besides the cost factor, automation and care coordination solutions also allows care providers to make timely interventions that facilitate proactive healthcare. By easing the data gathering, analysis and paperwork burdens, automation frees providers to spend more time offering superior patient care and driving better outcomes. In the end, this becomes the true value gained from value-based purchasing.
Get started on better value-based payment models today. Contact a reimbursement expert at SolvEdge Healthcare solutions today. Give us a shout.
From our humble beginnings as a healthcare start-up—to becoming a full-blown healthcare-exclusive digital transformation provider, our journey has been quite a remarkable one. Today, SolvEdge is a leading-edge Healthcare services and solutions provider—trusted by 450+ Hospitals, 3500+ Physicians and millions of patients across the globe.