Transforming Pediatric Scoliosis Care with Advanced Techniques
Align advanced imaging and outcome measures to optimize scoliosis correction and reduce surgical burden.
Transforming Pediatric Scoliosis Care with Advanced Techniques
Align advanced imaging and outcome measures to optimize scoliosis correction and reduce surgical burden.
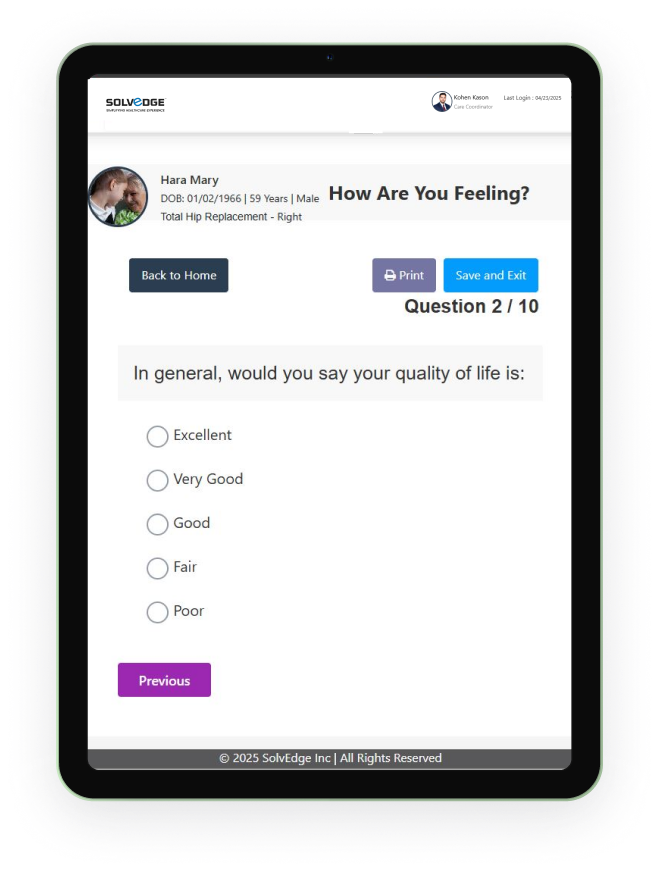
Tracking what truly matters
Understanding the pediatric scoliosis journey means going beyond the curve. By focusing on what children experience before, during, and after treatment, care teams are better equipped to act with precision and empathy. Leveraging patient-reported outcomes helps teams stay attuned to how young patients feel, function, and heal—aligning care with what matters most to children and their families.
Evaluates the patient's health-related quality of life (HRQoL) across domains like pain, function, self-image, and mental health specifically for scoliosis.

A broader measure assessing functional status and well-being in children with musculoskeletal conditions, including scoliosis.
Focuses on the patient's perception of their spinal appearance, which is a significant concern for many with scoliosis.
Although more commonly used for adult spinal conditions, it can assess the impact of scoliosis on a child's daily functional activities and disability.
Generic health status measures that assess overall physical and mental health, allowing for comparison with the general population.
Assesses breathing difficulties, which can be relevant for patients with significant thoracic scoliosis affecting lung function.
Powered suported by leading international healthcare service
Designed for growing spines
From early diagnosis to surgical correction, pediatric scoliosis care depends on adaptable tools made for children. These devices are crafted with growth, flexibility, and minimally invasive design in mind—allowing the youngest patients to thrive during and after their journey.

Pedicle Screws, Rods, Connectors
Outcome:
Stabilizes spine, corrects deformities like scoliosis, is best for adolescents (10-16) with significant curves. Improves the alignment and fusion.

Growth-Friendly Implants
Outcome:
Designed for younger children, these implants allow the spine to grow naturally while ensuring proper alignment and correction, reducing the need for multiple surgeries.

Anterior/Posterior Fixation Systems
Outcome:
These dual stabilization systems are effective for children of various ages, providing comprehensive spinal correction and long-term stability while accommodating growth.

Magnetically Controlled Rods
Outcome:
Non-invasive rod extension reduces surgeries for younger patients between ages 6–12.

Spinal Tethers
Outcome:
A dynamic option for adolescents, guiding the spine’s growth without fusion in kids aged 9+.

Vertebral Body Stapling Devices
Outcome:
Designed for mild curves in early stages, ideal for patients in pre-growth spurts.
Streamlined for lasting outcomes
Integrating Care Navigation with real-time PROMs has made the pediatric scoliosis care journey more connected, transparent, and patient-first—from the first consult through post-op care and beyond.
Personalized dashboards
help care teams proactively adjust treatment plans for each patient.
Family-centric care
education empowers decision-making and lowers anxiety across the care cycle.
Early identification
of complications through PROMs improves recovery speed and long-term wellness.
Seamless coordination
between specialties ensures no step is missed in the child’s care timeline.
Data-backed insights
refine next-gen tools with a focus on comfort, adaptability, and performance.
Increased transparency
in outcomes boosts trust and long-term adoption.
Real-time feedback
loops inform precision design updates and usage tracking.
Market readiness
is accelerated by aligning development with patient needs and clinical priorities.

Ready to Redefine Pediatric Spine Care?
Where innovation meets growing needs