Winning Under CMS TEAM: How Surgical Hospitals Can Protect Margin on Joint & Spine Bundles Without Sacrificing Outcomes
- SolvEdge
- Dec 22, 2025
- 5 mins read
The CMS TEAM bundled payments model launches January 1, 2026—mandatory for selected hospitals across key geographic areas. This five-year initiative holds facilities accountable for the full spine surgery episode of care and LEJR bundle optimization, from procedure through 30 days post-discharge. With target prices incorporating a CMS discount and quality adjustments, exceeding benchmarks means repayments; beating them unlocks shared savings.
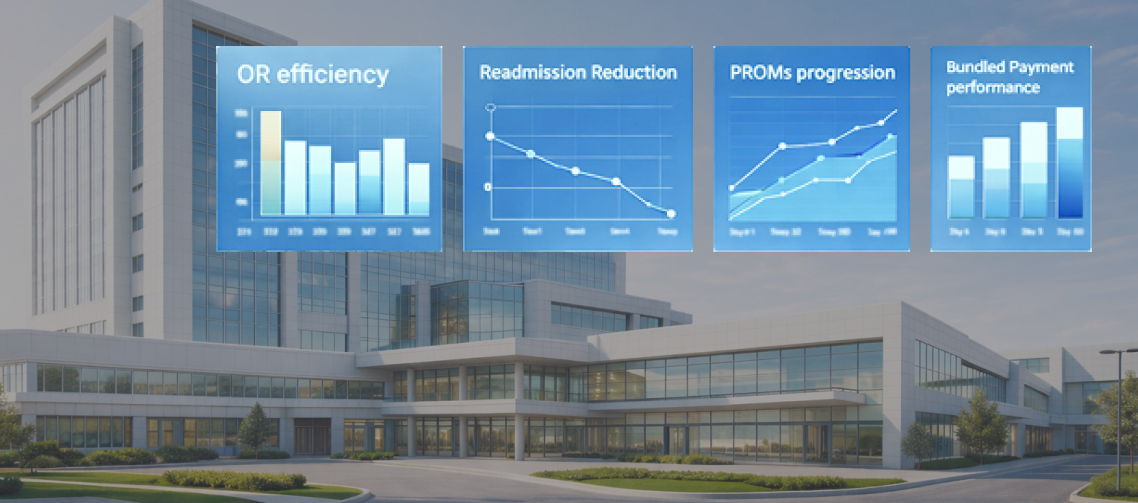
For orthopedic and surgical hospitals, this is the biggest shift since CJR. Orthopedic bundled payment strategy now demands precision across OR efficiency, pathway standardization, surgical readmission reduction, length of stay management joint replacement, and orthopedic PROM requirements. The winners? Those who integrate data across the episode without disrupting surgeon autonomy or patient experience. Here’s how leading systems are preparing for surgical hospital value based care success.
Understanding the TEAM Stakes for Joint and Spine Programs
TEAM covers high-volume episodes like lower extremity joint replacement (LEJR) and spinal fusion—procedures driving significant Medicare spend.
Key pressures:
Shorter episodes: 30 days post-discharge tightens focus on rapid recovery and complication prevention.
Quality-linked finances: Composite scores from readmissions, complications, and orthopedic PROM requirements directly scale rewards or penalties.
No more silos: Hospitals bear risk for post-acute spend (SNF, HHA, readmits).
One regional system already modeling TEAM benchmarks projects $1.2–2.8M annual swing per 500 episodes—purely from hospital episode analytics gaps.
Step 1: Standardize Pathways While Preserving Surgeon Alignment
Variation kills margins.
Leading hospitals deploy evidence-based protocols for implants, anesthesia, and pain management—reducing cost per case 8–14% without mandating one-size-fits-all.
Pre-op risk scoring → Flags SDOH and comorbidities for tailored plans.
Intra-op defaults → Opioid-sparing and goal-directed fluids as opt-out, not opt-in.
Post-op milestones → Early ambulation tied to discharge readiness.
Hospital episode analytics provide surgeon-specific dashboards showing cost, LOS, and outcomes—fostering buy-in through transparency, not top-down mandates.
Step 2: Master Length of Stay and Discharge Efficiency
Length of stay management joint replacement and spine cases is ground zero for savings.
Top performers:
Shift eligible LEJR to outpatient/23-hour observation.
Embed discharge planning at pre-op—matching patients to home health vs. SNF based on risk.
Use predictive tools to identify Day 0/1 discharge candidates.
A Midwest hospital cut average LEJR LOS by 0.9 days and post-acute spend by 18% through real-time analytics flagging delays.
Step 3: Drive Down Surgical Readmissions Through Proactive Monitoring
Readmissions remain the biggest controllable risk in TEAM.
Strategies proving effective:
Automated post-discharge check-ins for pain, wound issues, and red flags.
Remote mobility tracking for joint patients; neurologic checks for spine.
Closed-loop escalation—sub-threshold responses trigger nurse navigator outreach within 24 hours.
Facilities integrating these reduced surgical readmission reduction by 25–35%, directly boosting quality scores.
Step 4: Elevate PROMs Collection and Use
Orthopedic PROM requirements aren’t just compliance—they’re a quality multiplier.
CMS weights patient-reported outcomes heavily in composite scoring.
Best practices:
Start collection pre-op for baseline.
Automate timed surveys (Day 14, 30, 90) via patient-preferred channels (SMS/app).
Feed results into clinical dashboards for interval interventions.
One spine program lifted response rates from 58% to 92%—adding 0.4–0.6 points to their quality adjustment.
The Integrated Analytics Advantage
Success in TEAM hinges on hospital episode analytics that connect OR data, inpatient progress, post-acute utilization, PROMs, and claims—without replacing your EHR.
This unified view enables:
- Episode-level cost forecasting.
- Real-time variation alerts.
- Predictive risk for reconciliation planning.
Protect—and Grow—Your Margins Under TEAM
The hospitals thriving under CMS TEAM model rules won’t cut corners on care—they’ll illuminate them with data.